Cough is extremely common in children and usually gets better by itself with no specific treatment, although the cough often takes 2 to 3 weeks to disappear. Occasionally, children with a cough can develop a chest infection.
Symptoms of a chest infection:
- Prolonged fever
- Breathing faster than usual
- Using extra effort when breathing
- Being too breathless to feed (young children) or complete sentences (older children)
- Chest pain when breathing or coughing.
This guidance has been reviewed and adapted by healthcare professionals across the Black Country Integrated Care System.
Causes of cough
Most cases of cough in children (under 5 years of age) are caused by viral infections. Your child may also have a runny nose, cough or earache.
Treatment
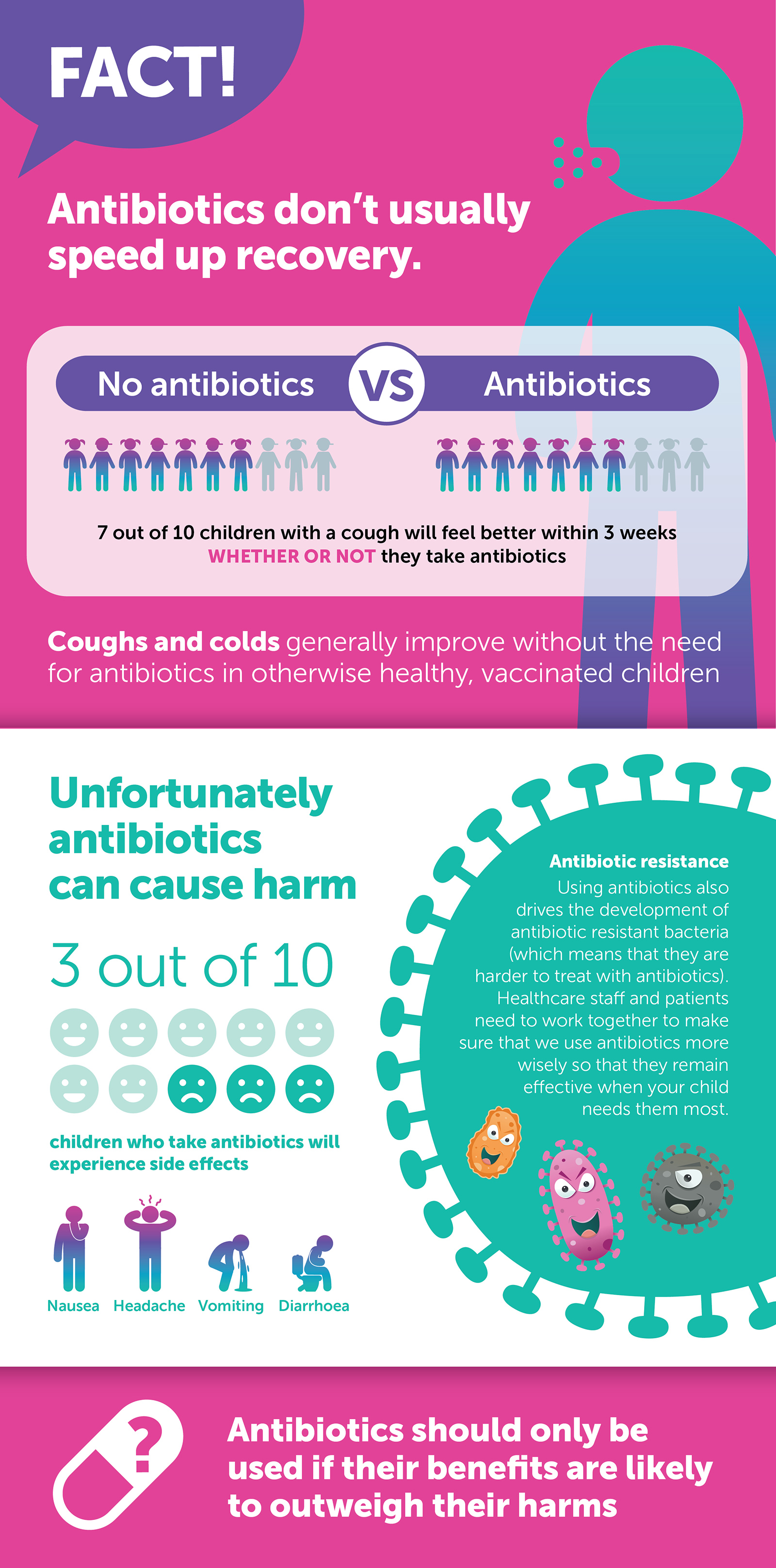
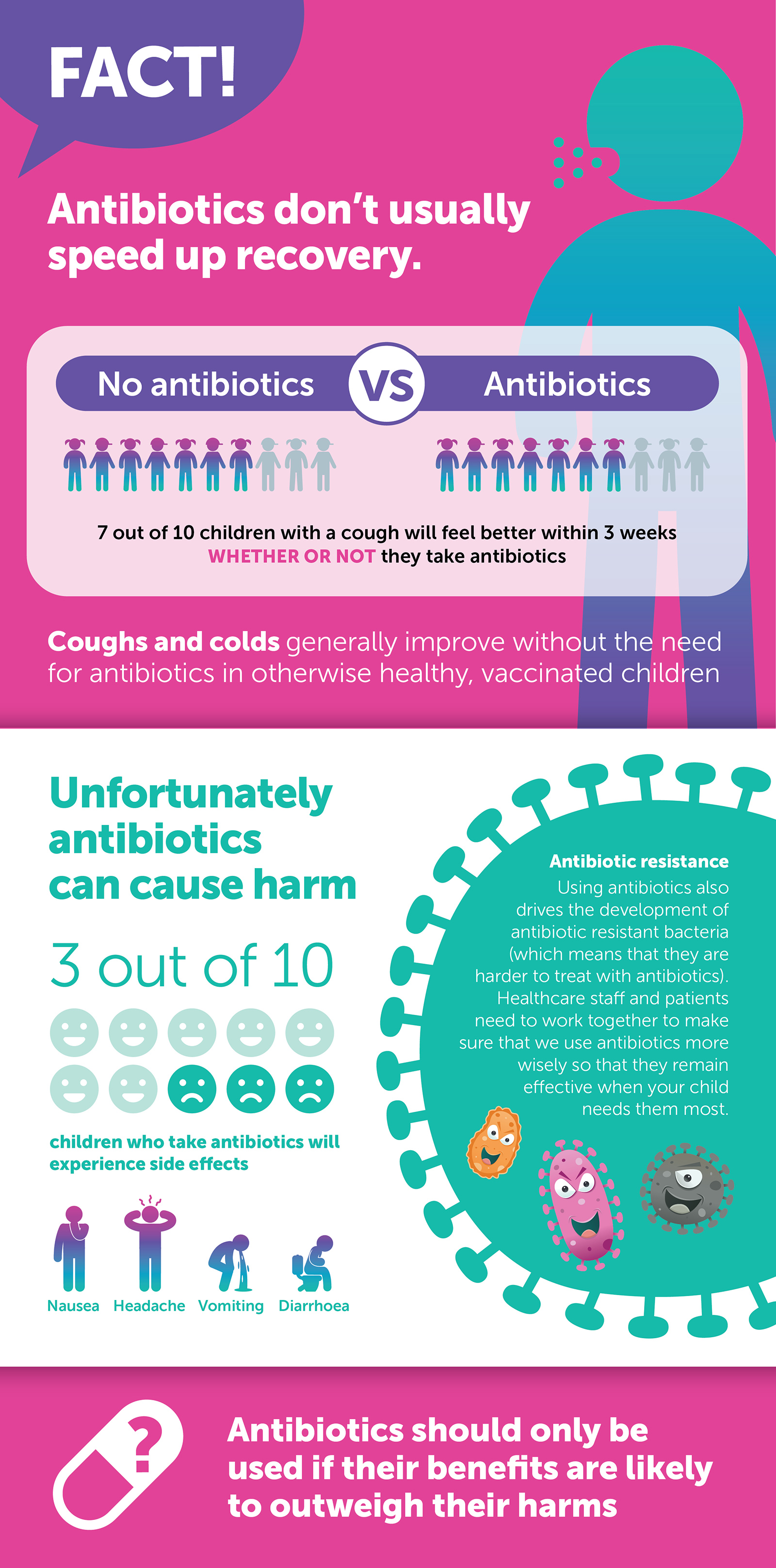
Most children with coughs/colds do not require treatment with antibiotics. Antibiotics rarely speed up recovery and often cause side effects such as rash and diarrhoea. They will also promote the development of antibiotic resistant bacteria in your child.
Antibiotics are usually only considered if your child has a high fever for more than 24 hours and is breathing faster than normal, plus using extra effort when breathing. If your child has a wheeze and difficulty breathing, they are very unlikely to benefit from antibiotics but may benefit from inhalers.
In addition, if your child has any amber or red features above, they will need to be urgently seen by a healthcare professional, who may decide that your child may benefit from additional treatment.
You can help relieve symptoms by:
- Giving your child paracetamol or ibuprofen if they have a fever
- Encourage your child to drink plenty of fluids.
It can take a few weeks for a child to fully recover from a cough. Children rarely cough up phlegm, but they are still clearing their chest. If you are worried that after an initial improvement, their cough is getting significantly worse, or not getting better after 4 weeks, you should take your child to see their GP. Most children make a full recovery from a chest infection with no lasting effects.
If your child is struggling to breathe, they need to be urgently seen by a medical practitioner and are likely to need treatment. If your child has Croup (hoarse voice, barking cough, noisy breathing), they will also need to be seen by a medical practitioner.
If your child has a runny nose and breathing difficulties, it is most likely that they have a condition called bronchiolitis. Most children with bronchiolitis get better by themselves with no specific treatment. Bronchiolitis is caused by a viral illness, so antibiotics are not helpful.
Symptoms of Bronchiolitis:
- Your child may have a runny nose and sometimes a temperature and a cough
- After a few days your child's cough may become worse and their breathing may get faster/more laboured
- As breathing becomes more difficult, your baby may not be able to take their usual amount of milk by breast or bottle
- Your child may vomit after feeding and you may notice fewer nappies than normal.
How long does bronchiolitis last?
- Most children with bronchiolitis will seem to worsen during the first 1-3 days of the illness before beginning to improve over the next two weeks. The cough may go on for a few more weeks
- Your child can go back to nursery or day care as soon as he or she is well enough (feeding normally and with no difficulty in breathing).
Prevention
It is not always easy to avoid catching these infections. However, good hygiene practices can prevent infections spreading:
- Wash your hands regularly and thoroughly
- Use a tissue when coughing or sneezing and put it in the bin
- Avoid sharing glasses or utensils with people who are unwell.
Feedback Question: Has the advice on this page helped you with a healthcare decision?